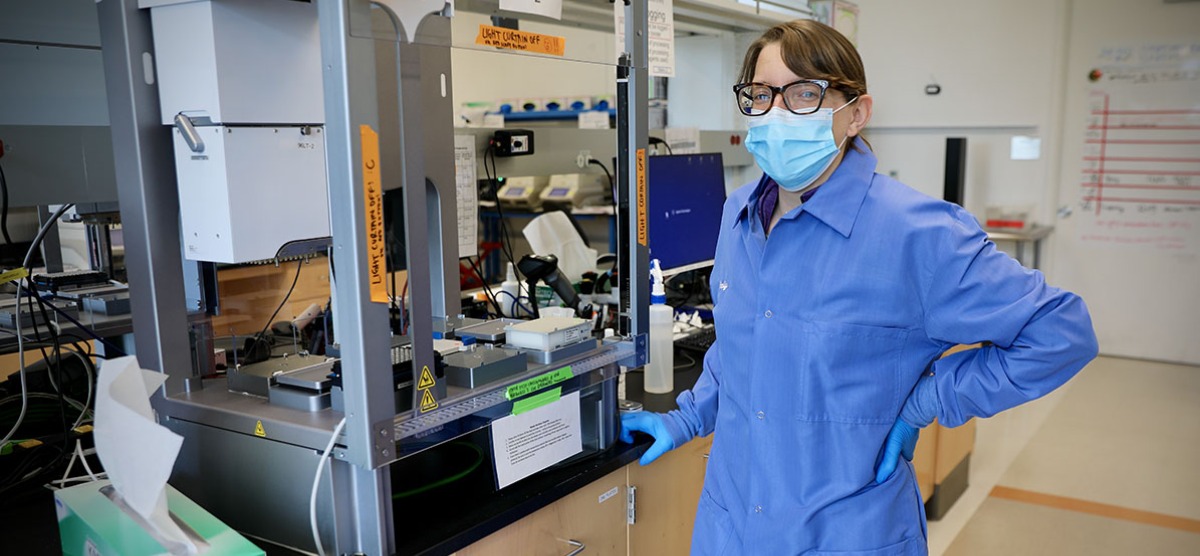
Emily Crawford '03 Leads COVID-19 Testing Project
In a span of eight days, Crawford transformed a research lab into a clinical diagnostics lab.
A researcher in the Chan Zuckerberg Biohub and faculty member at the University of California, San Francisco, Emily Crawford '03 focuses on developing next-generation methods for infectious disease diagnostics with a particular focus on antibiotic resistance detection in bacterial infections.
But, in early March, when California Governor Gavin Newsom issued an executive order that opened the way for research labs like the Biohub to perform clinical diagnostics, Crawford’s focus quickly shifted to making that transformation happen.
The Chan Zuckerberg Biohub is located in San Francisco, with a close affiliation with the medical school of the University of California, San Francisco (UCSF). “So, when the USCF clinical microbiology lab asked us to turn our facility into a COVID-19 diagnostic lab,” Crawford says, “Joe DeRisi, my boss and the Biohub co-president, was eager to say yes.”
With that, the Biohub’s COVID-19 Task Force, which Crawford leads, pivoted and, in eight days—“eight crazy days,” she calls them—transformed a research lab into a clinical diagnostics lab.
EIGHT CRAZY DAYS
The first order of business Crawford faced was creating an organizational structure and, to do so, meant drawing on her liberal arts background. “I didn't train for this in my Ph.D. program,” she says, “and it was an eye-opening experience to know how broad a skill set you need. All of a sudden, there’s an immediate human impact to what I’m doing. And I realized that I had absolutely nowhere near the bandwidth to do and organize everything myself. So the very first thing I did was to ask a colleague to be my co-lead.”
Plus, redundancy is critical because, as Crawford says, “You never know who might get sick.”
Together, they identified 13 different work teams that would be required—and two people to serve as co-leaders. “Then we started calling those people and asking if they were willing to be involved,” Crawford says. “And that was all within one day of the announcement.”
There was a facilities team to ensure that the lab space had the appropriate set-up—enough emergency power outlets, proper ventilation, appropriate freezer space, etc. A supply chain team worked the phones to secure everything needed for testing. There was a personnel team recruiting and overseeing the volunteer workforce, a regulatory team, a team for making the reagents used in the assay, a team for waste management to deal with the biohazard and chemical hazardous waste, and several teams devoted to developing the actual tests.
“Early on, one of the most critical teams was the regulatory team that worked side by side with UCSF’s main clinical lab to understand the legal and regulatory hurdles we needed to overcome,” Crawford explains. “We couldn't have done anything without that support every step of the way, walking us through how you do the validation, who you send the reports to, all that.”
And at the end of those eight crazy days, the lab got its validation, submitted an emergency use authorization to the FDA, and was ready to run more than 2,000 clinical tests a day.
“But then, we had a number of disheartening weeks when we were running less than 100 tests a day.” says Crawford. “Nobody in the Bay Area—or really the world—had enough nasal swabs.”
Within two weeks, that shortage was substantially alleviated, and the lab was processing about 1,000 tests a day. “We are very strict and regimented about PPE,” says Crawford. “We wear masks whenever we're in the building and, in the lab itself, lab coats and goggles. We have a laundry system to reduce the risk of exposure. We've contracted with the local market to provide individually packaged meals for lunch and, for anyone working at night, dinner.
"The biggest thing we've done for reducing exposure,” she explains, “is organizing our volunteers into four different squads and those four squads never interact with each other. So if there were to be an outbreak in one, we could isolate those people, and the other three would still able to function.”
THE CHALLENGE
To create a diagnostic lab, the three biggest challenges are acquiring instrumentation, reagents for running the equipment, and the people who run it.
For the Biohub, the first need—equipment—was answered by a host of Bay Area firms who were happy to donate equipment. “We had people driving all around—to UC Berkeley and companies in Silicon Valley—to pick up different automation instruments and PCR instruments that we needed,” Crawford says. “We used our networks and found everything we needed.”
On the reagents side, she explains, “we focused from day one on using reagents normally used only for research, not for clinical testing. So we contacted companies that hadn't yet been contacted, and we bought enough supplies to be able to process a total of 100,000 tests.”
The third piece—personnel—is largely composed of some 200 UCSF students and postdocs, researchers now serving as clinical lab technicians. “But again,” Crawford reports, “everyone throughout has been so happy to help and to be able to contribute.”
The challenge now, she says, is sustaining the work for the long term. “I’ve been running on adrenaline,” she says, “but now I’m trying to transition from the sprint phase to the marathon phase, because I know that this thing isn't going anywhere.”
More than three decades ago, in 1984, a new method of diagnosing infectious disease revolutionized the clinical world. Called PCR—polymerase chain reaction—it's the standard today for infectious disease diagnostics. The basis for PCR is thermal cycling, which involves rapidly changing the temperature of the reaction by heating it to the boiling point of water and then cooling it back down, back and forth, back and forth, 40 or 50 times over the course of an hour or so.
“We've been doing PCR tests for many decades,” says Crawford, “and that experience has given us a good understanding of what its limitations are, where it works, where it doesn't work, what the false positive and false negative rates are, and how to control those.”
LIFE B.C. (Before Coronavirus)
Crawford’s early career was focused on developing new diagnostic tools to vastly improve over PCR—high-tech, next-generation methods based on DNA sequencing that promised to provide a full profile of antibiotic resistance in a given infection. “Say someone has a streptococcus infection,” she explains, “using these high-tech protocols, we could see that it is resistant to antibiotics, X, Y, and Z, but not to A, B, or C. And then the doctor could prescribe one of those drugs.”
Over the past year or so, as she began interacting more with physicians and the people who actually work in clinical care, Crawford began to realize that the high-tech methods she was researching have limited real-world applications. “You can sit in a lab and work with your million-dollar instrumentation all you like,” she says, “but you're not going to get that to work on a scale that can be applied to enough people to address the antibiotic crisis.”
Instead, the future of diagnostics is going to be rapid, low-cost technologies. PCR meets one of those requirements—affordability—but, because it requires a centralized lab where the sample can be processed, turnaround times can be less than optimal.
So just before the pandemic broke out, Crawford had been starting to transition part of her group towards working on that problem, with the gene-editing technology CRISPR playing a lead role. “CRISPR is on the verge of being the biggest improvement in infectious disease diagnostics in 35 years,” Crawford says. “The promise of this technology, I believe, is that it will eliminate the lab setting and enable us to offer a home diagnostic test that's equivalent to a pregnancy test.
“When all this started, I thought, this is CRISPR’s moment. But then my colleagues and I had to decide whether it was going to be as reliable as the PCR technology we’ve been using for decades. And what we realized was that it’s just not quite there yet because, in its current state, CRISPR technology hasn’t been challenged to anywhere near the extent that PCR has.”
The scientist in her is a little rueful: “I would love to work with the shiny new toy that’s so much fun to play and work with,” she says. “But in the current crisis situation, it was clear that the only thing that made sense was to go with the tried-and-true PCR method.
“But if COVID had come along maybe a year from now,” she adds, “we might be talking entirely about CRISPR-based diagnostics.”
Photo credit: Michael Guilbert
Published on: 06/15/2020